For several years, abdominoplasty has only been covered for massive weight loss patients with significant amounts of redundant skin.
As of the 1st of July, 2022, a tummy tuck is covered by Medicare for those patients with significant rectus diastasis that have maintained a normal body weight.
Rectus diastasis repair is beneficial in patients having abdominoplasty surgery. Rectus abdominis muscle separation can cause abdominal weakness, back pain and urinary incontinence and make the abdomen appear bloated.
What is the new item number for tummy tuck or abdominoplasty?
The item number is 30175.
Full criteria to qualify for the item number as seen on the Medicare website are listed below.
It is important to note that you must have:
At least 3cm of rectus muscle separation confirmed by an ultrasound
Have moderate pain or discomfort at the site of the separation during functional use and/or low back pain or urinary symptoms
The symptoms need to have failed to respond to non-surgical treatments such as physiotherapy
Your last pregnancy must have been completed 12 months ago
You can only have one abdominoplasty per lifetime under this item number.
The full criteria on the Medicare website are as follows:
Radical abdominoplasty, with repair of rectus diastasis, excision of skin and subcutaneous tissue, and transposition of umbilicus, not being a laparoscopic procedure, where the patient has an abdominal wall defect as a consequence of pregnancy, if:
(a) the patient:
(i) has a diastasis of at least 3cm measured by diagnostic imaging prior to this service; and
(ii) has symptoms of at least moderate severity of pain or discomfort at the site of the diastasis in the abdominal wall during functional use and/or low back pain or urinary symptoms likely due to rectus diastasis that have been documented in the patient’s records by the practitioner providing this service; and
(iii) has failed to respond to non-surgical conservative treatment including physiotherapy; and
(iv) has not been pregnant in the last 12 months
Applicable once per lifetime
Is the item number different for massive weight loss patients undergoing tummy tuck or abdominoplasty?
Yes it remains the same as before. It is 30177
In order to qualify there must have been significant weight loss which has been stable for six months.
The skin excess need to be much that it interferes with the activities of daily living
The skin excess causes a skin condition such as fungal rashes which have failed 3 months of conservative management.
The full Medicare criteria are as follows:
(a) there is intertrigo or another skin condition that risks loss of skin integrity and has failed 3 months of conventional (or non surgical) treatment; and
(b) the redundant skin and fat interferes with the activities of daily living; and
(c) the weight has been stable for at least 6 months following significant weight loss prior to the lipectomy
How will I benefit by having private health insurance for my abdominoplasty?
All patients are encouraged to obtain insurance before larger procedures such as an abdominoplasty as it covers overnight hospital stays, surgical time and there are some rebates for surgical and anaesthetic fees. The most significant part of this surgery are hospital costs which are charged at an hourly rate in uninsured patients.
Wait times to have surgery are one year from the date of starting an insurance policy. Although it seems like a long time, it is much better to wait this time as the cost savings are significant. As well, in the rare event of any complications requiring a longer hospital stay or longer surgery, insurance will cover a significant proportion these additional costs if medically necessary.
It is important to check your insurance level covers the item number 30175 or 30177 if you qualify when taking out private insurance.
Some lower levels of cover may not cover abdominoplasty surgery so it is not only important to take out insurance, however the correct tier of private cover as well.
Which aspects of my abdominoplasty surgery will not be covered?
If additional liposuction (such as VASER liposuction) is required to achieve a uniform transition of results in the flank area, this surgical time is not covered by insurance as it is cosmetic.
There are gaps for the surgical fees and anaesthetic fees and there is only a partial rebate for these. The surgical costs are time based and as abdominoplasties vary in size and complexity and how much liposuction will be done. It is not possible to provide an accurate quote without seeing the area.
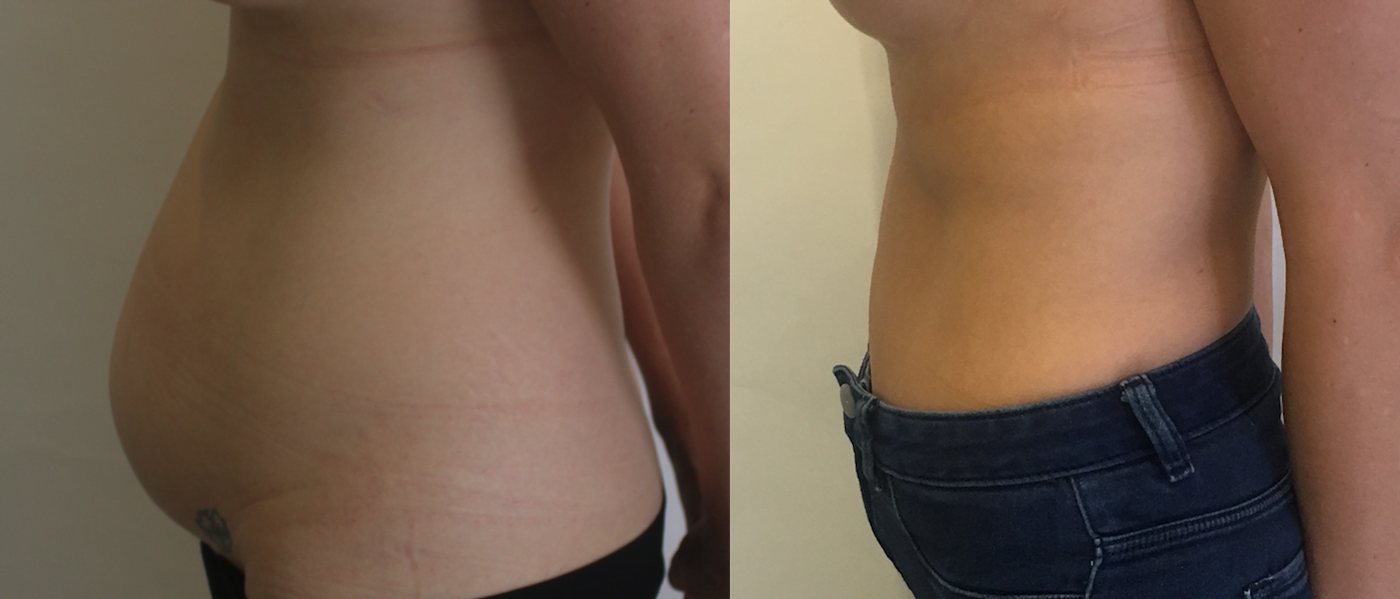
View the abdominoplasty before and after gallery
Disclaimer: All plastic surgery or invasive procedures carry risks.
Click here for more information about abdominoplasty
Surgical results and recovery vary depending on the individual patient.
Although an actual patient at one year post-operatively in the image, there is no guarantee that your results will be the same or similar to this result. Surgical results and recovery vary depending on the individual patient.
The content on this page is general in nature and does not constitute medical advice.
Before proceeding with any surgery, you should seek a consultation by an appropriately qualified health practitioner.